AITA for asking my aunt to not bring her kids when she comes to see us?
Life can sometimes deal us an unfair hand, especially when grief and loss collide with family disagreements. In this heartrending case, a 16-year-old brother shares the struggle of watching his 17-year-old sibling, Danny, face the final weeks of a devastating battle with metastasized bone cancer.
With hospice care now at home and emotions running high, Danny’s last wishes—centered around minimizing stress during his final days—are clashing with family expectations and painful past memories. It’s a time when every word and action feels magnified, and the importance of honoring personal comfort becomes paramount.
The setting is heavy with sorrow, yet it’s also a call for compassion and understanding. While family members gather to say goodbye, the focus must remain on making Danny’s remaining time as peaceful as possible.
Amidst tearful confrontations and harsh words, one sibling has taken it upon himself to advocate for Danny’s wishes, even if it means ruffling the feathers of relatives who seem unable to see past their own grief. This story asks a difficult question: How do we honor the needs of a dying loved one when everyone else seems overwhelmed by their own pain?

‘AITA for asking my aunt to not bring her kids when she comes to see us?’
Navigating the emotionally charged terrain of end-of-life care is a challenge for even the most prepared families. When someone as young as Danny faces hospice care, the focus shifts from battling illness to prioritizing comfort, dignity, and the patient’s specific wishes. As families struggle to cope with grief, the need for clear communication and steadfast advocacy becomes more crucial than ever. It’s not merely about managing symptoms but about tailoring the environment to support the patient’s emotional well-being during their final moments.
One key element in such situations is the recognition that hospice care is about enhancing the quality of life rather than prolonging suffering. In the words of renowned palliative care expert Dr. David Casarett, “Palliative care is not about giving up; it’s about focusing on what matters most: comfort, dignity, and quality of life.”
This sentiment resonates deeply when the patient explicitly states a need for fewer disruptions—even if it means asking relatives, particularly young children, to postpone their visits. It is a stance that prioritizes Danny’s fragile state over the natural but sometimes overwhelming impulses of extended family to gather.
The complexity of family dynamics in a hospice setting can often lead to conflict, as personal needs and grief intermingle with longstanding issues. In cases like Danny’s, where past trauma and current health crises overlap, setting boundaries is not a rejection of love but an essential part of care.
Experts advise that in moments of extreme vulnerability, the wishes of the patient should take precedence, even if that means difficult conversations and temporary estrangements. By prioritizing Danny’s mental and physical comfort, his family can help ensure that his final days are spent in as much peace as possible.
Moreover, open dialogue is key. Health care professionals, including hospice social workers and palliative care teams, stress the importance of involving everyone in discussions about care boundaries. They remind us that while the impulse to gather and share grief is natural, it must be balanced against the patient’s expressed needs.
When the environment becomes too chaotic, it can intensify pain and distress. In this light, the call to limit certain visitors—like young children who may not grasp the gravity of the situation—can be seen as an act of compassion and protection.
Ultimately, this case underscores a broader lesson in palliative care: the importance of tailoring the end-of-life experience to honor the patient’s voice. Even amid familial strife and differing opinions, the true measure of care lies in how well we listen to and respect the wishes of those nearing the end of their journey.
Here’s what the community had to contribute:
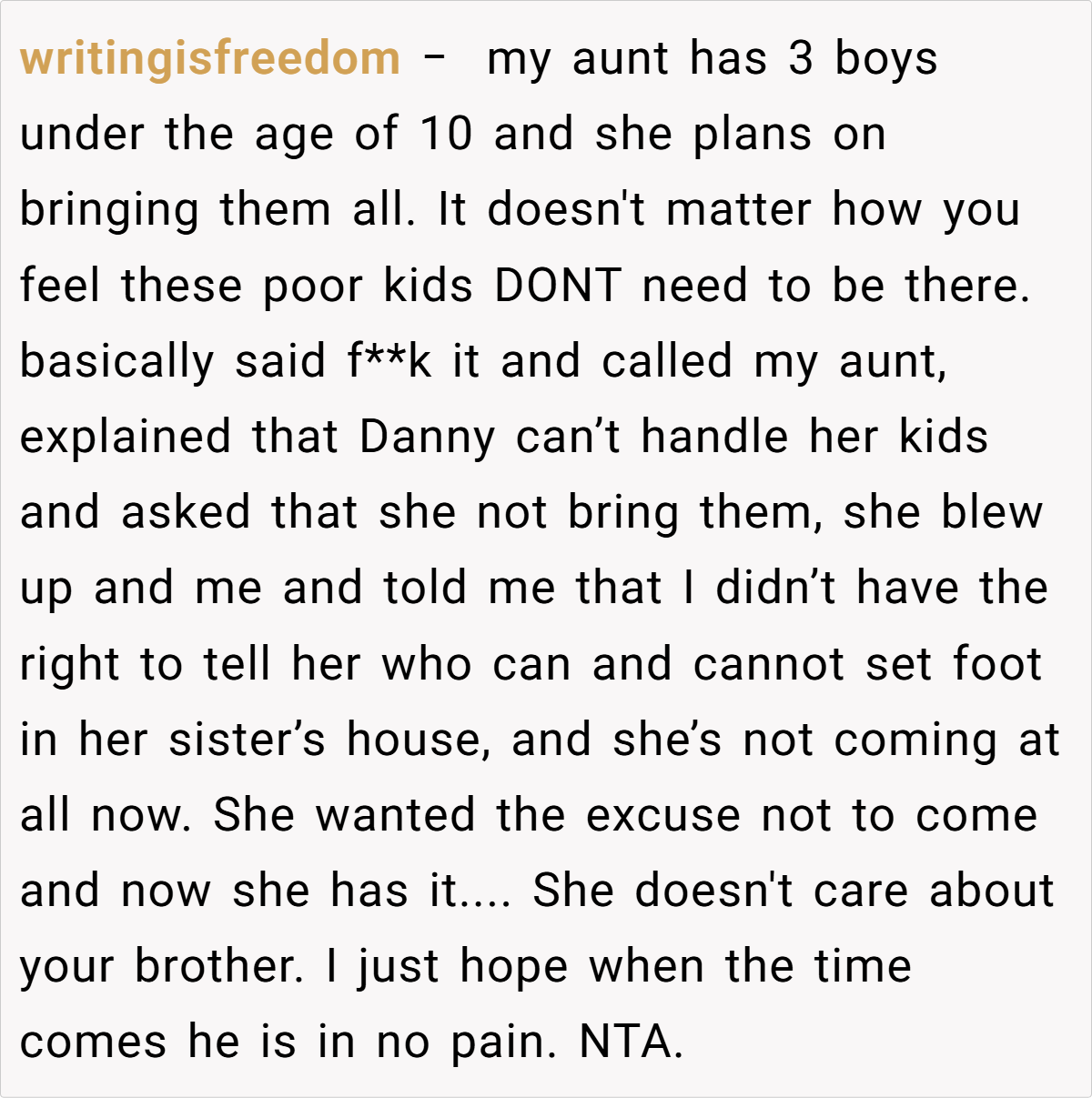
The Reddit community has rallied around the narrator with heartfelt support and clear guidance. Many comments emphasize that in moments like these, the priority must be the comfort and dignity of the patient. They argue that if family members cannot abide by Danny’s wishes—even if it means skipping out on a final farewell—they must accept that boundaries are essential. The responses range from empathetic advice to stern reminders that sometimes, protecting a loved one means making tough decisions.


In conclusion, when facing the imminent loss of a loved one, the emotional landscape can become a battleground of conflicting needs and grief. While family is meant to be a source of comfort, sometimes honoring a patient’s last wishes means drawing firm boundaries—even if it alienates some.
What do you think? How should families balance the urge to gather and grieve with the pressing need to respect a dying loved one’s request for peace? Share your thoughts and experiences in the comments—let’s discuss how to find compassion in the midst of such heartache.